Smallpox of monkeys
In recent years, we have witnessed outbreaks of rare infectious diseases, and one of these is monkey pox.
What is monkey pox?
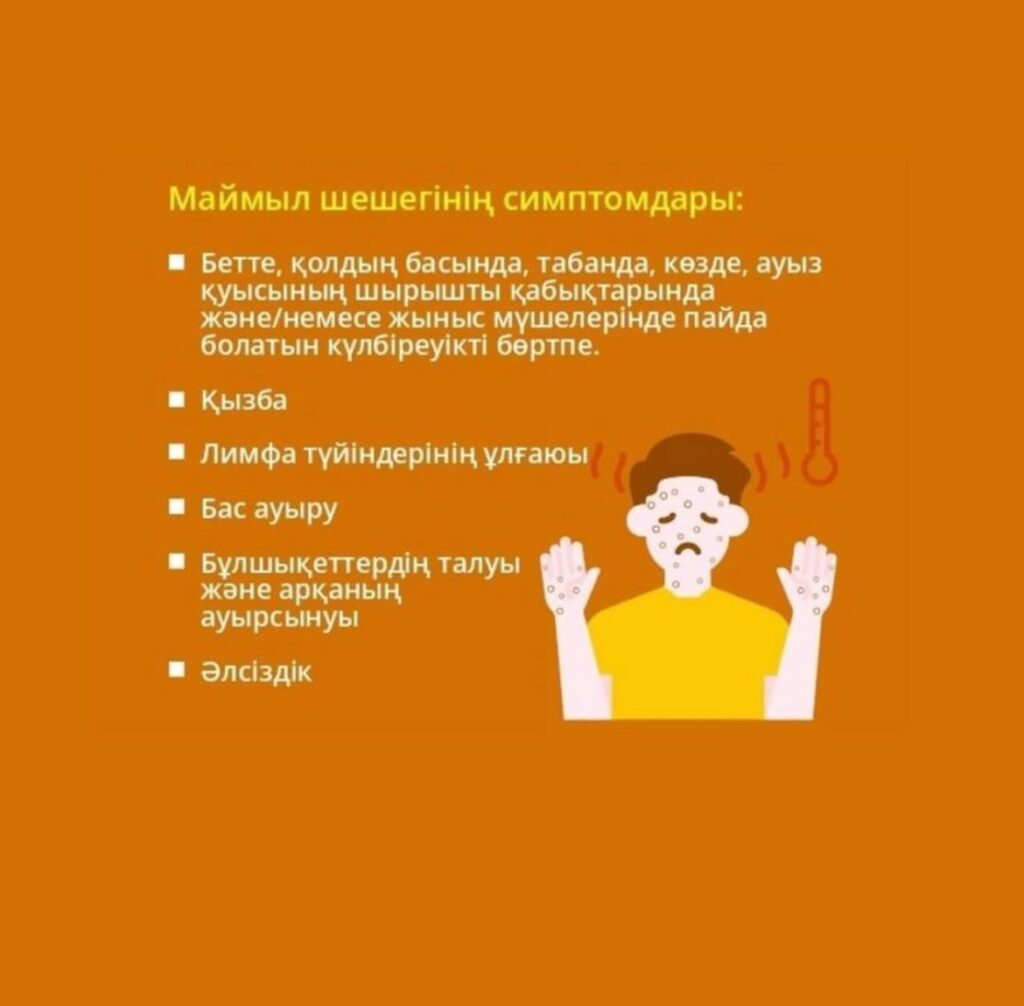
Monkey pox is a viral infection transmitted from animals to humans, and then from person to person. The main symptoms include:
– Fever
– Headaches and muscle pains
– Enlargement of lymph nodes
– The appearance of a characteristic rash and blisters
How is it transmitted?
Transmission of the virus occurs through close contact with an infected person, his biological fluids or objects used by the sick person (for example, towels, clothes).
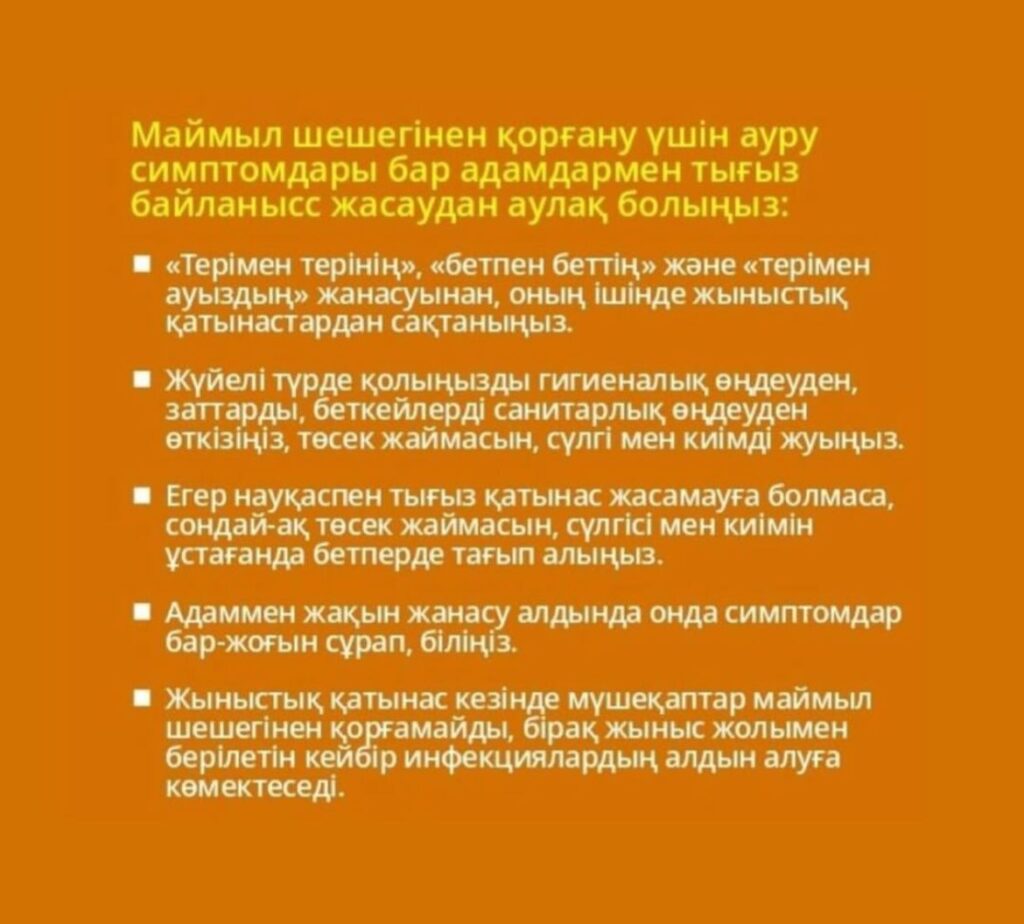
How to protect yourself?
– Avoid close contact with people who have symptoms.
-Observe hygiene: wash your hands, use disinfectants.
– Follow the WHO news and recommendations.
What to do if you get sick
If symptoms appear, consult a doctor immediately. Early detection and isolation of patients help prevent the spread
of the virus.
Chickenpox — forms, symptoms, first aid.
Chickenpox is an acute viral disease manifested by papular-pustular skin lesions and signs of general intoxication. It is more common in childhood. The older the patient, the higher the risk of systemic complications.
Causes of chickenpox
The causative agent of the disease is human herpevirus of the third type. This is the chickenpox virus, which also causes shingles. There are eight known types of herpesviruses. Transmission of the pathogen occurs mainly by airborne droplets. It enters the body after contact with the mucous membrane. You can get infected:
when communicating with a patient;
after staying in public places where the infected person could be;
through things (dishes, towels).
The infection can also penetrate through the placenta — from the mother to the fetus. In theory, the varicella zoster virus can travel in the wind, but the pathogen quickly dies outside the body.
Symptoms of chickenpox
The incubation period lasts about two weeks. At this time, the microorganism actively multiplies in the body and does not manifest itself in any way. Further, symptoms occur as you move from one stage to another:
Prodromal
It begins in children with a slight malaise, in adults — more severe, with a rise in temperature to 40 degrees. At the same time, the first rashes appear.
Active.
The rash spreads throughout the body. In a child, these are episodic pimples concentrated in the upper part of the body, in adults, a generalized form with damage to the entire skin is possible.
Recovery.
The last bubbles burst and dry up, new ones do not form.
The recovery period can take a long time. There are no rashes anymore, but the immune system is weakened, so there remains a risk of complications.
Forms of chickenpox
The forms of the disease are distinguished depending on the severity of its course and the severity of symptoms. In general, chickenpox can be typical and atypical.
A typical one can occur in one of three forms:
1. Easy. It is typical for an early age. The child experiences almost no discomfort. The disease manifests itself in rashes or spots, but they do not burst or itch.
2. Medium-heavy. The rash is actively spreading, papules itch, transform into pustules, burst and become crusted. At the same time, the temperature rises slightly, headache and cough are possible.
3. Heavy. Rashes appear not only on the skin, but also on the mucous membranes. The temperature rises noticeably, accompanied by vomiting, confusion.
Acne with chickenpox in an atypical form may be absent altogether. Instead, spots or signs of damage to small vessels appear.
What does chickenpox look like?
It is impossible not to notice it — it has pronounced external symptoms. However, not everyone can immediately distinguish chickenpox from other infectious diseases accompanied by rashes. This can be done by analyzing what the rash looks like.
It goes through several transformations:
A speck;
papule is a protruding nodule;
A pustule is a vial with liquid contents;
an ulcer is a burst and dried bubble.
If the pustules burst themselves and heal, there are no traces on the skin. However, if they are combed and damaged ahead of time, scars may form. There is also a risk of introducing bacteria into wounds or exacerbating the course of the disease by re-entering the pathogen through the blood.
Chickenpox usually begins with rashes on the face, scalp, neck or back. It spreads to the chest, abdomen and limbs as the course becomes more complicated.
First aid
As soon as the first signs of chickenpox appear, the patient must be isolated. It becomes contagious even at the prodromal stage, but it is difficult to suspect an infectious disease. Quarantine usually lasts 21 days.
When chickenpox begins, measures should be taken to ease its course:
Relieve itching. Antihistamines help in this.
Ensure hygiene. It is important to keep the child’s hands clean, change clothes and bed linen frequently to avoid bacteria getting into burst pustules.
Observe the drinking regime. The infected person needs a lot of fluids.
Take care of psychological comfort. All the thoughts of a teenager can be directed at how he looks. It is important to convince him that there will be no scars.
Common signs of intoxication are eliminated as in acute respiratory viral infections. Antipyretic or nonsteroidal anti-inflammatory drugs will help.
How to treat chickenpox?
Symptomatic treatment of chickenpox is reduced to skin care in the rash area. Papules and pustules are treated with an antiseptic solution of brilliant green or potassium permanganate. If a rash appears on the mucous membrane, zelenka and potassium permanganate should not be used. A 3% solution of hydrogen peroxide is suitable for disinfection.
If the disease begins with a strong rise in temperature, it can be assumed that it will occur in a moderate or severe form. This is a difficult test for the body, therefore, an antiviral drug should be taken on the first day. Doctors usually recommend famciclovir orally. However, it is not suitable for children with weakened immune systems and pregnant women. They are prescribed acyclovir orally or intravenously.
Possible complications
Chickenpox in adults is not only more pronounced symptoms and treatment, but also a high risk of complications, some of which can be fatal:
chickenpox pneumonia;
thrombocytopenia, which leads to blood thinning;
acute neurological disorders of a reversible nature;
epilepsy;
meningitis;
Varicella encephalitis with damage to the myelin sheaths of the brain and spinal cord.
Nonspecific complications of chickenpox are associated with bacterial infection of pustules. Festering wounds not only look unsightly. It is possible to develop an abscess (inflammation of tissues with subsequent deformation of the affected area), phlegmon (inflammation that spreads indefinitely) or even sepsis (blood poisoning).
Prevention
The main preventive method is vaccination. There is a method of passive immunoprophylaxis. This is a method in which a specific immunoglobulin is administered. This method is shown:
Newborns whose mothers contracted chickenpox between 4-5 days before giving birth;
Unvaccinated or untreated patients who have significant cellular immunodeficiency. It can be primary or acquired. The method is indicated for such patients after contact with those who have already had smallpox.
After using the method, post-exposure pharmacological prophylaxis is also carried out with special pharmacological preparations provided for these cases.
Polio/Acute flaccid paralysis!

Polio (the name comes from the words “polio” — gray, “myelon” — spinal cord) is a viral infectious disease that affects the nervous system and causes complete paralysis.
The syndrome “Acute flaccid paralysis” refers to any case of acute flaccid paralysis in a child under 15 years of age, including Guillain-Barre syndrome, or any paralytic disease, regardless of age, with suspected polio, as well as all cases of paralytic polio.
Children who have not been vaccinated against this infection (who have received less than 3 polio vaccinations), or vaccinated with a violation of the vaccination schedule, are at the greatest risk of polio infection in the case of importation of wild polio virus.
The main signs of polio
The virus enters the human body through the mouth and multiplies in the intestines. The initial symptoms are fever, lethargy, headache, vomiting, pain in the limbs, neck, back, weakness of the muscles of the arms and legs. One in 200 cases of infection leads to irreversible paralysis (usually of the legs). Of these paralyzed patients, 5-10% die as a result of paralysis of the respiratory muscles.
After the first symptoms of the disease appear, the virus continues to be excreted in faeces, 1 gram of which contains up to 1 million infectious doses. Therefore, the main importance is the fecal-oral mechanism of transmission of infection through fecal-contaminated water and food. In epidemic foci, people can become infected by airborne droplets.
The incubation (latent) period of polio is at least five days, up to a maximum of a month, on average two weeks. The further course of the disease will depend on the human immune system.
The source of infection in polio can be both a sick person and an asymptomatic virus carrier that secretes the virus with nasopharyngeal mucus and feces.
Polio prevention
Polio can be prevented by vaccination (specific prevention).
Polio vaccinations are included in the national preventive vaccination calendar.
Polio prevention follow the rules of personal hygiene:
- wash your hands thoroughly with soap before each meal, after visiting public places, coming home from the street;
- do not buy products in places of unauthorized trade;
- wash fruits and vegetables thoroughly before use under running water and rinse with boiled water;
- do not use water from non-drinkable water sources (wells, fountains, springs, lakes, rivers, etc.) for drinking purposes, use only boiled or bottled water and factory packaged beverages.
- do not swallow water during water procedures and bathing in open reservoirs.
- during the trip, eat at certain food outlets where products of guaranteed quality of industrial production are used, you should not eat products of traditional national cuisine that have not undergone guaranteed technological processing, as well as purchased in places of street trade.
Polio vaccinations, made on time and according to the rules, will help prevent your child and those around you from having a serious and dangerous disease like polio!
We strongly recommend that you do not self-medicate when the first signs of the disease appear in your child! It is necessary to immediately seek medical help (to call a doctor from a polyclinic at the place of residence or, in case of serious condition, an ambulance team and follow their recommendations). Remember that the combination of rehabilitation methods allows you to get a good therapeutic effect only if you receive timely treatment. Pathology is dangerous for its complications, including:
– reduction in the size of the affected limb or body part due to the fact that the muscles are atrophied;
– hardening of the muscles in the affected area (contracture);
– hardening of the joints.
By vaccinating a child, you protect him from infectious diseases.
By refusing vaccinations, you risk the health and life of your child.
Remember that the disease is easier to prevent than to treat!
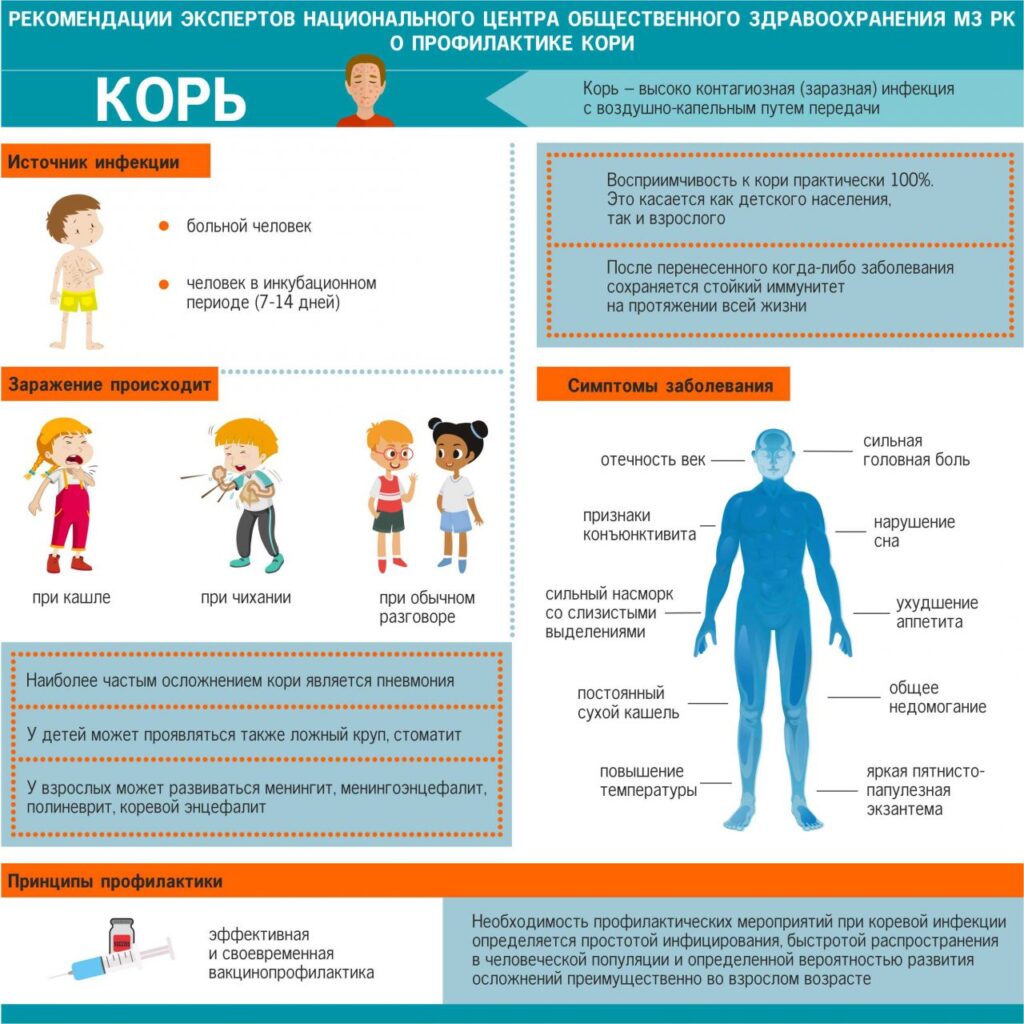
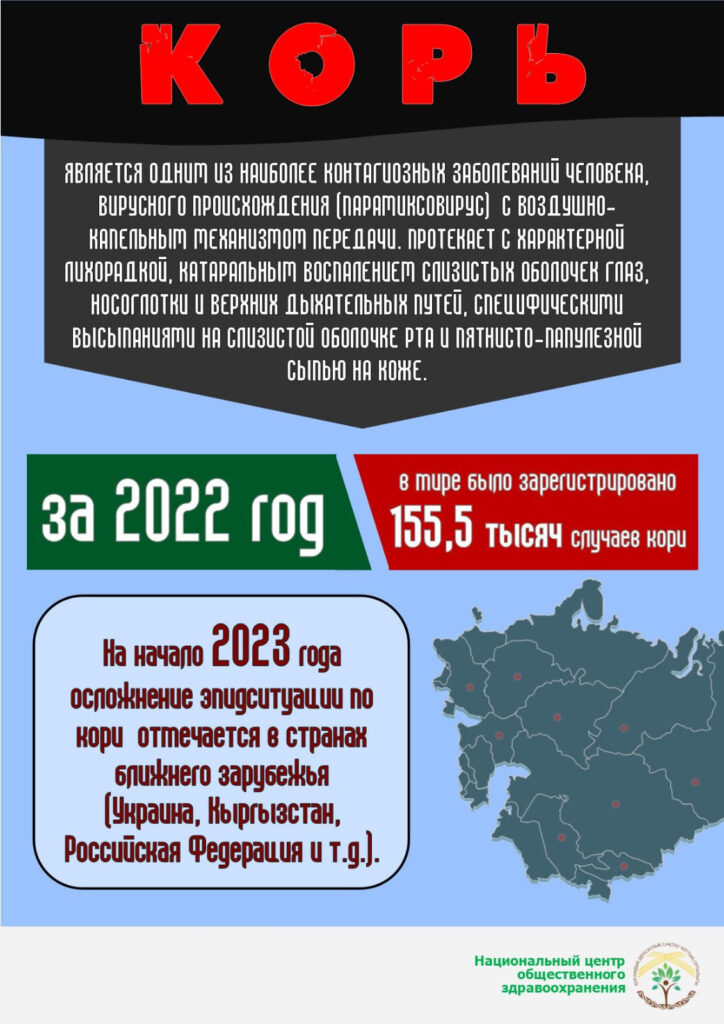
Etiology. Clinic. Treatment. Measles prevention.
Measles is an acute infectious disease characterized by general intoxication, inflammatory phenomena from the mucous membranes of the eyes, nasopharynx, upper respiratory tract, and a characteristic rash.
The causative agent of measles is a virus. It is not stable in the external environment: it dies at room temperature for 5-6 hours.
The only source of infection is a sick person. The spread of the virus occurs when sneezing, coughing, talking with droplets of saliva. If a person has not had measles or has not been vaccinated against this infection, then after contact with the patient, infection occurs in almost 100% of cases. The measles virus has a very high volatility. The virus can spread through ventilation pipes and elevator shafts – children living on different floors of the house get sick at the same time. Unlike children, adult patients rarely have a rough, barking cough, stenotic breathing, at the same time bronchitis, tracheitis with dry cough are characteristic. In rare cases, catarrhal phenomena are accompanied by asthenia and dyspeptic disorders, joint pain. At the same time, the so—called measles enanthema appears on the mucous membranes of the lips, cheeks and gums, on the conjunctiva-Belsky-Filatov-Koplik spots, towering whitish-yellowish “dots” above the surface of the mucous membrane. This is an important early diagnostic sign of measles, lasting 2-3 days. From the beginning of the peak period, when a rash appears, the patient’s condition worsens, intoxication increases. The temperature is kept at high numbers. During the rash, catarrhal symptoms, lacrimation, photophobia, cough, laryngitis persist, and puffiness of the face increases. Measles in adults often occurs with early damage to the nervous system in the form of drowsiness, a sharp headache. The exanthema is characterized by a papular-spotted character, a tendency to merge, and the stage of appearance: the first elements of the rash are found on the face and behind the ears, during the day the rash covers the entire face, neck, and partially the upper part of the chest. It is characterized by filling the nasolabial triangle with a rash. On the 2nd day, the exanthema spreads to the trunk and proximal parts of the limbs, and on the 3rd day – to the entire surface of the limbs. The fading rash acquires a bluish hue, then turns into light brown spots. The period of rash extinction, or pigmentation period, begins. It lasts from 3 to 8 days. The extinction of the rash is accompanied by a fine bran-like peeling of the skin of the face and trunk. Peeling lasts 5-7 days. It is most pronounced on the face, palms and soles. Depending on the nature of the rash and the severity of the disease, there are separate clinical forms of measles: mild, moderate, severe and mitigated (erased). Measles is observed in children who have received prophylaxis with measles immunoglobulin. Complications of measles are possible in the form of pneumonia, otitis media, stomatitis, thrombophlebitis, encephalitis, myocarditis, glomerulonephritis, strepto- and staphylodermatitis, furunculosis. The cause of complications can be both the measles virus and the secondary microbial flora. Complications are observed more often in patients weakened by previous diseases, suffering from allergic diseases. The immunity of patients who have had measles is quite stable. Repeated measles cases are rare. For the second time, people who have had measles at an early age, who have had it in a mitigated form, and who have received antibacterial therapy for measles (!!!) become ill. A strict proof of measles disease is either the isolation of the measles virus from the patient, or serological confirmation of the presence of the virus in the body – the appearance of specific class M antibodies or an increase in the titer of class G antibodies in the blood serum. Drug treatment is pathogenetic and symptomatic in nature. In case of fever and intoxication, non–specific anti-inflammatory drugs are prescribed; in case of cough, expectorants and mucolytics, etc. Antibiotics are not prescribed for uncomplicated course!!! Complications are treated according to their localization and etiology.
Measles prevention
Vaccination is a decisive, affordable and effective method of fighting infection. In accordance with the National Calendar of Preventive Vaccinations, routine vaccination of children against measles is carried out at the age of 12 months and again at 6 years old. And adults aged 18-35 who have not been ill, have not been vaccinated or have no information about measles vaccination. Vaccination is necessary for all those who have come into contact with a measles patient who do not have reliable information about a measles vaccination or measles in the past. Measles vaccines create reliable immunity that lasts for more than 20 years. Vaccination prevents the development of measles, even if it is carried out during a worsening epidemic situation.
Meningococcal infection, clinic, diagnosis and medical care at the PHC and NSR stage

Meningococcal infection is an acute infectious anthroponous disease caused by the bacteria Neisseria meningitidis, transmitted by airborne droplets and characterized by a variety of clinical manifestations: from nasopharyngitis and healthy carrier to generalized forms in the form of purulent meningitis, meningoencephalitis and meningococcemia with damage to various organs and systems.
The causative agent of meningococcal infection is Neisseria meningitidis, gram-negative diplococcus
Symptoms of meningococcal infection
It takes from 1 to 7 days between infection and the appearance of the first symptoms.
The disease can occur in the form of nasopharyngitis, and with reduced immunity and serious chronic diseases, there is a risk of purulent meningitis (inflammation of the meninges), meningoencephalitis (inflammation of the membranes and substances of the brain) and sepsis.
The symptoms depend on the age and general condition of the body:
In young children, meningococcal infection is manifested by frequent regurgitation, monotonous screaming (“brain scream”), inadequate reaction to light, touch, noise. The child does not eat well or refuses breast/formula. There are fluctuations in body temperature, swelling and pulsation of the large fontanel. A specific “cocked trigger” pose is characteristic, in which the child throws back his head.
In adolescents and adults, signs of meningitis are repeated vomiting, unrelated to food intake and not bringing relief, confused consciousness. I’m worried about headaches and muscle aches. The temperature rises, an unusual reaction develops to light and touch — anxiety, irritation. Bending the head causes pain, which causes the patient to take a forced position.
The rash appears when an infection occurs in the form of meningococcal sepsis. Elements on the skin in the form of hemorrhages, irregular shape, pale pink with a bluish tinge, dense, rise above the skin, do not disappear when pressed. They are located on the lower part of the arms, legs, and buttocks. In severe cases, the rash elements spread to the torso and face.
Possible complications
The consequences of the disease are hydrocephalus, epilepsy, hearing problems, deterioration of cognitive functions, damage to the nervous system, amputation of fingers.
Some forms of the disease have a lightning course: within a day, the patient may die. In case of damage to the meninges, meningitis is fatal in 20% of cases.
Long-term rehabilitation is required during recovery.
Treatment
The main method of therapy is the use of antibacterial drugs. Symptomatic treatment is also used.
Contact persons are prescribed antibacterial therapy and emergency vaccination for preventive purposes.

Prevention of meningococcal infection
Vaccination against meningococcal infection is a reliable way to prevent the severe course of the disease and its consequences.
Routine vaccination of children is carried out with the Menactra vaccine, which contains 4 serotypes (varieties) of the bacterium. Vaccination provides long-term protection.
Before vaccination, the child is examined by a pediatrician. The specialist examines the medical history in detail, excludes contraindications to the procedure, and makes an individual vaccination plan.
Vaccines are stored in compliance with all sanitary standards. After vaccination, the baby is under the supervision of a healthcare professional for 30 minutes. Only after that, the mother and the child go home.